Sex Worker Health Checks at Gladstone Road Medical Centre
Inclusive, confidential & sex-positive care in Brisbane
I believe that sex work is work - and every worker deserves access to healthcare that is safe, respectful and free from judgment.
Our clinic offers confidential, comprehensive health checks designed specifically for people working in the sex industry. Whether you’re full-time, part-time, online, in-person, independent, in clubs, or working in adult content creation — your health and wellbeing matter here.
👌What makes our clinic different?
We provide a warm, sex-positive and affirming approach, with doctors who understand the needs of sex workers. That means:
✔ Non-judgemental care
✔ Inclusive of all gender identities, bodies, and sexualities
✔ Highly confidential medical records
✔ Longer appointments so you’re never rushed
✔ Support tailored to your work and your goals
Your privacy comes first. We never disclose your occupation to anyone else.
🔍 What’s included in a Sex Worker Health Check?
We offer a full range of sexual and general health services tailored to your needs. You don’t always need an examination, and tests can be self collected
🧪 Routine STI Screening
Chlamydia
Gonorrhoea
Syphilis
HIV
Hepatitis A, B & C
Rectal, throat, vaginal or penile swabs based on the type of work you do
Sexual health certificates
💉 Vaccinations & Preventative Care
Hepatitis A & B vaccines
HPV (cervical cancer & genital wart prevention)
PrEP & PEP consultations (HIV prevention)
🌼 Reproductive & General Sexual Health
Cervical screening (Pap smear)
Pregnancy testing & options counselling
Contraception (including IUD & Implanon)
Menopause and menstrual support
⚧ Gender-Affirming & Holistic Care
Hormone monitoring (oestrogen, testosterone, blockers)
Trans and gender-diverse care
Mental health support and referrals
💸 Pricing
Sex worker health checks at our clinic are privately billed, to ensure you have the time, space and privacy you deserve. This allows us to offer longer appointments, without rushing your concerns or your care. You’ll always know fees upfront, and Medicare rebates may apply depending on the appointment type.
📌 Who can book a sex worker health check?
Anyone working in the sex industry, including:
Independent workers
Brothel or massage workers
Strippers, dancers & club workers
Porn / OnlyFans / adult content creators
Digital or online workers (cam, custom videos, sexting, phone)
Part-time, casual or occasional workers
💬 No shame. No stigma. Just healthcare.
Healthcare should never be stressful or judgmental. At Gladstone Road Medical Centre, we see you as a person first — not as a stereotype or a risk category. Your consultation is a space where you can ask questions, get support, and make informed decisions about your body and your work.
📞 Book your appointment - 07 3844 9599
🌈 Gladstone Road Medical Centre
🏥 38 Gladstone Rd, Highgate Hill, Brisbane
📅 Regular and follow-up appointments available
🔐 Confidential, inclusive, sex-positive healthcare
👉 Call to book or visit HotDoc to make an online appointment.
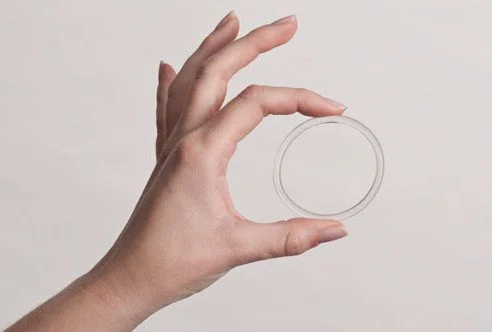
The NuvaRing: A “set and forget” alternative to the pill — now on the PBS
If you’ve ever found it hard to remember your pill every day, you’re definitely not alone. Between busy mornings, travel, and life in general, it’s easy to miss a dose. For years, the main alternatives were long-acting options like the IUD or implant — great for some, but not for everyone.
Now there’s another option getting more attention: the NuvaRing, a small, flexible ring that sits comfortably inside the vagina and releases hormones steadily over the month. And from 1 November 2025, it’s finally being added to the Pharmaceutical Benefits Scheme (PBS) — meaning it will now be much more affordable.
What actually is the NuvaRing?
Think of it as the “monthly version” of the pill. It contains the same types of hormones — oestrogen and progestogen — but instead of taking them orally, your body absorbs them directly through the vaginal wall. You insert the ring yourself (it’s soft and flexible, about 5 cm across), leave it in for three weeks, then remove it for one week — during that week you usually get a light withdrawal bleed. After that, you pop in a new one. Some people choose to skip periods by skipping the ring-free week, and putting the new one in early.
That’s it — no daily reminders, no fuss.
Why do some people love it?
The biggest drawcard is convenience. You only have to think about your contraception once a month, not every morning. It’s also a good option if you’ve had issues with nausea or gastrointestinal absorption from the pill — because the hormones don’t go through your digestive system. Periods often become more predictable, lighter, and less painful. And when you decide to stop, fertility typically returns quickly — usually within a few weeks.
If used correctly, the vaginal ring is 99.5% effective. With real life use, it can be less effective (93%), for example if you forget to take it out or put it back on time.
What about comfort or side effects?
Most people can’t feel the ring once it’s in place, and neither can their partner. Some might notice it at first, but this usually settles after the first cycle or two.
Side-effects are similar to those of the combined oral contraceptive pill — things like breast tenderness, mild nausea, bloating, or mood changes. These are often short-lived. As with any oestrogen-containing method, there are a few health conditions that make it unsuitable (for example, migraines with aura, clotting disorders, or smoking over the age of 35). That’s something we’d check carefully before prescribing.
The good news: it’s finally affordable
Until now, NuvaRing users have been paying the full private price — often more than $270 per year.
From 1 November 2025, the ring will be listed on the PBS, bringing the cost down to $31.60 per script (or $7.70 if you have a concession card). From 1 January 2026, the price will drop further to $25 per script as part of the Federal Government’s cheaper medicines initiative.
It’s a huge step toward giving Australian women and gender-diverse people more accessible contraceptive choices.
Who might find it a good fit?
NuvaRing tends to suit people who:
Want a reliable hormonal method but don’t want an implant or IUD
Find remembering a daily pill difficult
Prefer something reversible with quick return to fertility
Don’t mind handling their own contraception in a comfortable, private way
The bottom line
The NuvaRing isn’t new internationally, but for many Australians, it’s flown under the radar — largely because of cost and lack of awareness. With its PBS listing from 1 November 2025, that’s set to change. If you’re curious about trying the ring, or wondering how it compares to your current method, it’s worth chatting through your options. As with all contraception, the best choice is the one that fits your health, lifestyle, and comfort level.
Barrier to abortion access
Barriers to Termination of Pregnancy in Australia: Cost, Access, and the Importance of Affordable, Local Care
Access to safe and legal abortion is a fundamental part of reproductive healthcare, yet many people across Australia still face significant barriers to termination of pregnancy — particularly when it comes to cost, geography, and service availability. These obstacles can delay care or prevent access altogether, especially for people experiencing an unplanned pregnancy.
If you are exploring your pregnancy options, read more here.
1. Cost and Financial Insecurity
Even though medical termination of pregnancy (MTOP) is partially covered by Medicare, the out-of-pocket costs for abortion can be prohibitively high. In many private clinics across Australia, a medical abortion can cost anywhere from $250 to $600 or more. For people who are unemployed, studying, caring for others, or in financial distress, this creates a major barrier to timely access.
2. Geographic Isolation
People living in rural and remote areas of Australia face unique challenges when seeking an abortion service. There may be no local providers, and accessing a clinic could require significant travel, accommodation, and time off work or study — all of which add to the emotional and financial burden. Even within cities like Brisbane, some suburbs lack accessible services.
3. Limited Provider Availability
Not all GPs provide medical abortions, and referral pathways can be unclear or fragmented. Patients are sometimes told that their doctor "doesn't do that here" without being given clear information on where to go next. Delays in accessing care can reduce the available options, particularly for medical abortion which is only offered up to 9 weeks’ gestation.
4. Stigma and Privacy Concerns
Although abortion is legal, abortion stigma remains a real concern for many people, particularly in smaller or more conservative communities. Fear of being judged, concerns about confidentiality, or even past negative experiences with the healthcare system can stop someone from seeking help.
5. Misinformation and Confusion
Many people are unaware of their legal rights when it comes to abortion in Queensland and may not know that telehealth abortion is an option. Confusion around gestational limits, the difference between medical and surgical abortion, and concerns about safety or side effects may cause unnecessary anxiety and delay.
Low-Cost Medical Abortion in Brisbane — In Person or Via Telehealth
To help address some of these barriers, I now offer low-cost medical termination of pregnancy in Brisbane at Gladstone Road Medical Centre, located in Highgate Hill. This service includes:
A thorough consultation and bulk-billed follow-up care
A $25 gap fee or bulk billing available on request
Access to care in person or via telehealth, anywhere in Queensland*
Whether you're seeking abortion care in Brisbane or need telehealth abortion services from a more rural* area, I aim to provide respectful, inclusive, and affordable support. No referral is required.
If you're experiencing an unplanned pregnancy and want to discuss your options, you can book online at mitchkrosch.com or contact Gladstone Road Medical Centre directly. Everyone deserves timely, compassionate reproductive care — without financial or geographic barriers.
*You must be within two hours drive of an emergency department, in case of a complication.
10 Facts About Endometriosis
1. Endometriosis affects 1 in 9 people assigned female at birth.
Endometriosis is a chronic inflammatory condition estimated to affect around 1 in 9 people assigned female at birth by age 44 in Australia. It can have profound impacts on quality of life, including pain, fatigue, fertility concerns, and impacts on work and relationships.
📚 Source: Australian Institute of Health and Welfare. Endometriosis in Australia: Prevalence and hospitalisations
2. It’s more than “just bad periods.”
While period pain is common, the pain of endometriosis is often chronic, disabling, and can occur outside of menstruation. Dismissing it as “normal” can delay diagnosis and care.
📚 Source: Endometriosis Australia. Understanding Endometriosis
3. Pain during sex, or while going to the toilet can be a sign.
Endometriosis lesions can affect pelvic organs, leading to pain with intercourse (dyspareunia), bowel movements, or urination, especially during menstruation.
📚 Source: World Health Organization. Endometriosis fact sheet (2023)
4. It often starts in the teenage years.
Symptoms of endometriosis can begin soon after the onset of periods (menarche), but many teens are dismissed or misdiagnosed, increasing the emotional and physical toll.
📚 Source: American College of Obstetricians and Gynecologists. Endometriosis in adolescents
5. Diagnosis can take up to 7 years.
On average, people with endometriosis wait 6.5 to 7 years for a diagnosis due to normalisation of symptoms and lack of awareness among healthcare providers.
📚 Source: AIHW. Endometriosis in Australia
6. You don’t need visible endometriosis to have severe pain.
Pain severity doesn’t always correlate with how much disease is seen on imaging or laparoscopy. Even microscopic or deep infiltrating lesions can cause disabling symptoms.
📚 Source: Royal College of Obstetricians and Gynaecologists. Endometriosis: diagnosis and management
7. Fertility problems are common—but not inevitable.
Up to 50% of people with endometriosis may experience infertility, but many still conceive naturally or with assisted reproductive technologies. Early management and support matter.
📚 Source: ASRM. Endometriosis and infertility: A committee opinion
8. Hormonal treatments don’t cure it—but can help.
Medications like the pill, progestins, and GnRH analogues may reduce pain and slow progression, but they do not eliminate endometriosis. They are part of a toolbox—not a fix.
📚 Source: NICE Guidelines. Endometriosis: diagnosis and management (NG73)
9. Surgery can help—but isn’t always the answer.
Laparoscopic excision can reduce pain and improve fertility—but not all patients benefit, and recurrence is possible. Surgery is most effective when combined with long-term care.
📚 Source: Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG). Endometriosis
10. There is support—and you deserve care.
You’re not alone. Advocacy groups, specialist GPs, pelvic physios, and psychologists can all help. Early recognition and a multidisciplinary approach can make a huge difference.
📚 Source: Jean Hailes for Women's Health. Managing endometriosis
For amazing Queensland based support, look at qendo.org.au.
Struggling With Low Iron? You Might Need More Than Just Tablets
Disclaimer: This article is for general information only and does not replace personalised medical advice. If you’re concerned about fatigue or iron deficiency, please speak to your GP.
Feeling tired all the time? You’re not alone. Fatigue is one of the most common reasons people visit their GP. And one of the biggest causes? Low iron, also known as iron deficiency. Many people — and even some doctors — don’t realise just how much iron deficiency can affect your energy levels, mood, and quality of life. So let’s break it down.
What Does Iron Actually Do?
Iron is essential for your body to make red blood cells. These red blood cells carry oxygen around your body — to your brain, muscles, and every other organ. If your iron levels stay low for long enough, you might become anaemic — which means you don’t have enough haemoglobin or red blood cells to carry oxygen efficiently. Anaemia can cause serious health problems. But here’s the important part: you don’t have to be anaemic to feel awful.
There’s strong evidence now that iron deficiency alone — even without anaemia — can cause significant fatigue.
Why Do People Become Iron Deficient?
There are a few common reasons iron levels drop:
Not enough iron in your diet – Red meat is the richest source of iron, but plant-based eaters need to pay special attention to getting enough iron through other foods (like legumes, leafy greens, and fortified cereals).
Losing iron through bleeding – This could be heavy periods or, more concerningly, bleeding from the bowel.
Pregnancy and breastfeeding – These are times when your iron requirements go up significantly.
If you’ve been told you’re low in iron, your doctor should help you figure out why — because that helps determine the best treatment approach. Sometimes a dietitian can help you boost your intake, and sometimes managing bleeding (such as with an implanon or IUD) can reduce iron loss.
Iron Tablets: A Good First Step
If you’re iron deficient, your doctor might recommend trying iron supplements first. And here’s a handy tip: taking iron every second day actually helps your body absorb it better.
For many people, iron tablets are effective — but not for everyone.
Some people:
Don’t absorb iron well through the gut
Can’t tolerate the side effects (like nausea, constipation or stomach pain)
Or just never get their levels up despite months of tablets
But What If Tablets Don’t Work?
This is where things get frustrating. Too often, people try iron tablets, feel unwell, and then… give up. They live with ongoing fatigue, brain fog, poor sleep, low mood, or worsening menstrual symptoms — all linked to iron deficiency.
But it doesn’t have to be that way.
If tablets don’t work (or just aren’t realistic for you), there’s another option: iron infusions.
Iron Infusions: An Underrated Game Changer
Iron infusions are safe, fast, and often life-changing. They deliver iron directly into your bloodstream through a drip, bypassing the gut. Most people feel significantly better within a few days to a few weeks.
So why aren’t they used more?
Some doctors are unsure of the guidelines
Others are concerned about rare side effects
Cost and access can be a barrier for many patients
And sometimes… we just don’t talk about it enough
But for the right person, an iron infusion can mean the difference between just getting through the day — and actually enjoying it.
What’s Involved in an Iron Infusion?
A small cannula is placed into a vein in your arm
The iron is infused slowly over 15–30 minutes (sometimes longer)
You’ll be monitored for a short time afterwards to make sure you feel okay
There is a very small risk of an allergic reaction, but this is extremely rare, especially with the newer iron formulations we use today. Some people get a temporary metallic taste, or feel a bit achey afterwards. Most people tolerate infusions really well.
The Bottom Line
If you’ve been told you have low iron, and you’re still feeling exhausted — don’t settle. Ask your doctor if an infusion might be right for you. You deserve to feel better, and iron deficiency is both common and treatable.
Sometimes a simple iron check — and the right treatment — can completely turn things around.
Ready to Feel Better?
If you’re struggling with fatigue, low mood, or poor concentration and wondering if iron could be part of the picture — book an appointment to chat about testing and treatment options, including infusions.
You don’t have to keep running on empty. Let’s figure it out together.
Bacterial vaginosis breakthrough study
A recent groundbreaking study has unveiled a significant shift in our understanding and treatment of bacterial vaginosis (BV), a common vaginal infection affecting nearly one in three women. Traditionally, BV was viewed as an imbalance in vaginal bacteria, not classified as a sexually transmitted infection (STI). However, new research indicates that BV can be sexually transmitted, and treating both female patients and their male partners simultaneously leads to higher cure rates and reduced recurrence.
Understanding Bacterial Vaginosis
BV occurs when there's an overgrowth of certain bacteria in the vagina, disrupting the natural balance. This imbalance can cause symptoms like a fishy odour, unusual discharge, and discomfort, though some women may not experience noticeable signs. If left untreated, BV can lead to complications, including an increased risk of acquiring other STIs and issues during pregnancy.
The Landmark Study
Researchers from Monash University and Alfred Health conducted a study involving 164 heterosexual couples, where women diagnosed with BV were treated alongside their male partners. The men received a combination of oral antibiotics and topical antibacterial cream. The results were striking: BV recurred in only 35% of women whose partners were also treated, compared to 63% in the control group where only the women received treatment.
Implications of the Findings
This study challenges the previous notion that BV is not sexually transmitted and highlights the importance of treating both partners to prevent reinfection. The findings suggest that men can harbor BV-associated bacteria and transmit them back to their female partners, leading to recurrence. By treating both individuals, the cycle of reinfection can be broken, offering more effective management of BV.
What This Means for You
If you or someone you know is dealing with recurrent BV, it's essential to consider the role of sexual partners in treatment. Here are some steps to take:
Consult Your Healthcare Provider: Discuss the possibility of simultaneous treatment for both you and your partner. This approach may significantly reduce the chances of BV returning.
Practice Safe Sex: Using condoms can help reduce the transmission of BV-associated bacteria between partners.
Maintain Vaginal Health: Avoid practices that can disrupt the natural balance of bacteria in the vagina, such as douching or using scented products.
Looking Ahead
While this study marks a pivotal step in understanding BV's transmission and treatment, further research is needed to develop comprehensive prevention strategies and update clinical guidelines. In the meantime, awareness of the potential for sexual transmission and the benefits of treating both partners can empower individuals to take proactive steps toward better vaginal health.
Vodstrcil, L. A., Plummer, E. L., Fairley, C. K., Hocking, J. S., Law, M. G., Petoumenos, K., Bateson, D., et al. (2025). Male-Partner Treatment to Prevent Recurrence of Bacterial Vaginosis. New England Journal of Medicine, 392(10), 947-957. https://doi.org/10.1056/NEJMoa2405404
Which IUD should I choose?
If you're thinking about getting an intrauterine device (IUD) for contraception, you might be wondering which one is best for you. In Australia, there are three main types of IUDs available: Mirena, Kyleena, and the Copper IUD. Each has its own benefits and drawbacks, so let's break it down to help you decide.
If you're thinking about getting an intrauterine device (IUD) for contraception, you might be wondering which one is best for you. In Australia, there are three types of IUDs available: Mirena, Kyleena, and the Copper IUD. Each has its own benefits and drawbacks, so let's break it down to help you decide.
Kyleena size comparison
There are three IUDs to choose from in Australia:
Mirena - levonorgestrel 52mg
Kyleena - levonorgestrel 19mg
Copper IUD
Mirena —
Mirena can stay in place for up to 8 years.
Mirena is larger than Kyleena but similar in size to the Copper IUD.
The Mirena is inserted in a similar way to the other IUDs. Some people experience cramping during and after insertion, but pain relief options can help.
Mirena is over 99% effective at preventing pregnancy.
Best suited for:
Mirena is a good choice for both people who have had children (parous) and those who haven’t (nulliparous). Because it's slightly larger, some people who haven’t had children may find insertion more uncomfortable. If we can time the insertion during or just after your period, the insertion tends to be more straightforward. It is also one of the best methods to reduce or stop heavy menstrual bleeding or irregular cycles.
Risks:
Irregular bleeding or spotting in the first 4-6 months
Possible hormonal side effects like mood changes or breast tenderness ( though this is much less likely than other hormonal methods such as The Pill)
Small risk of the IUD moving or being expelled
Very low risk of infection at the time of insertion
Kyleena —
Kyleena can stay in place for up to 5 years.
Kyleena is smaller than Mirena and the Copper IUD, making it a good option for people who prefer a smaller device.
Kyleena is over 99% effective at preventing pregnancy.
Because it is smaller, Kyleena may be slightly easier and more comfortable to insert than Mirena, especially for people who haven’t had children.
Best suited for:
People who have never been pregnant (nulliparous) because of its smaller size. It is also a good option for those who want a lower dose of hormones than Mirena.
Risks:
Irregular bleeding or spotting, especially in the first few months
Possible hormonal side effects (probably less than with Mirena)
Small risk of the IUD moving or being expelled
Very low risk of infection at the time of insertion
Copper IUD —
The Copper IUD can stay in place for 5 to 10 years, depending on the type.
The Copper IUD is similar in size to the Mirena.
The procedure is the same as with hormonal IUDs, and some cramping is normal during and after insertion. The Copper IUD does not contain hormones, which can be a benefit for those who want a completely non-hormonal option.
The Copper IUD is over 99% effective at preventing pregnancy. It can also be used as emergency contraception if inserted within 5 days after unprotected sex.
Best suited for:
The Copper IUD is suitable for both parous and nulliparous people. However, those who already experience heavy or painful periods may find that the Copper IUD makes this worse.
Risks:
May cause heavier, longer, or more painful periods
Small risk of the IUD moving or being expelled
Very low risk of infection at the time of insertion
Which One is Right for You?
If you want long-term contraception with light or no periods, Mirena might be the best choice.
If you want a smaller IUD with fewer hormones, Kyleena is a great option.
If you prefer a hormone-free method, the Copper IUD is your best bet.
All IUDs are highly effective, long-term contraception options, but the right one for you depends on your body and preferences. Talk to your doctor to discuss what suits you best!
What to Expect During an IUD Insertion
Thinking about getting an IUD (Intrauterine Device) but feeling a bit nervous about the procedure? You’re not alone! Many people have questions about what to expect, and it’s completely normal to have some concerns. The good news is that IUD insertion is a quick, routine procedure that provides long-term, highly effective contraception.
Thinking about getting an IUD (Intrauterine Device) but feeling a bit nervous about the procedure? You’re not alone! Many people have questions about what to expect, and it’s completely normal to have some concerns. The good news is that IUD insertion is a quick, routine procedure that provides long-term, highly effective contraception. In this post, we'll walk you through what happens before, during, and after the insertion so you can feel informed and prepared.
What is an IUD?
An IUD is a small, T-shaped device that sits inside the uterus to prevent pregnancy. There are two main types:
Hormonal IUDs (Mirena or Kyleena) - These release a small amount of progestogen, which thickens cervical mucous and thins the lining of the uterus.
Copper IUDs - These are hormone-free and work by creating and environment that is toxic to sperm.
Both types are over 99% effective and can last between 5-10 years, depending on the type you choose.
Before the Appointment
1. Consultation with Your Doctor
Before getting an IUD, you’ll have a chat with your doctor to discuss your medical history, contraception needs, and which IUD is best for you. They may also perform a pelvic exam or STI screening to ensure there are no infections before insertion.
2. Preparing for the Procedure
Here are a few tips to make your appointment smoother:
Take ibuprofen and paracetamol about 30-60 minutes before your appointment to help with discomfort.
Eat a light meal beforehand to avoid feeling lightheaded.
Bring a pad or panty liner in case of light spotting afterward.
Ideally, have someone drive you to and from the appointment (in case you feel a little crampy or lightheaded afterwards).
During the insertion
The actual procedure only takes a few minutes and happens in a standard GP or clinic room. Here’s how it works:
1. Positioning & Examination
You’ll lie on an examination table (similar to a Pap smear position). The doctor will insert a speculum to gently open the vagina, allowing them to see the cervix.
2. Measuring the Uterus
The cervix is gently grasped, which can cause a pinching feeling (although a lot of people don’t feel anything). A small instrument called a sound is used to measure the depth of your uterus to ensure proper placement of the IUD. This may cause a brief cramping sensation.
3. Inserting the IUD
The IUD is introduced via a thin tube, which is inserted through the cervix into the uterus. Once in place, the arms of the IUD open up, and the tube is removed. The doctor will trim the IUD strings, which stay inside the vagina so the IUD can be checked or removed later.
4. All Done!
The entire process usually takes 5-10 minutes.
After the procedure
1. How Will I Feel?
Mild to moderate cramping (like period pain) is common for the first few hours.
Light spotting or irregular bleeding may occur for a few weeks.
Some people feel totally fine right away, while others may prefer to rest for a little while.
2. What to Watch For
While complications are rare, contact your doctor if you experience:
Severe pain or heavy bleeding
Fever or unusual discharge (possible infection)
Inability to feel the IUD strings (which may indicate it has moved)
3. When Does It Start Working?
Hormonal IUD: If inserted within the first 7 days of your cycle, it's effective immediately. Otherwise, use backup contraception for 7 days.
Copper IUD: Works immediately, even as emergency contraception.
Getting an IUD is a safe, quick, and effective way to prevent pregnancy, and for many people, the benefits far outweigh any temporary discomfort. If you’re feeling anxious, remember that your doctor is there to support you and make the experience as comfortable as possible. If you have any concerns before or after the procedure, don’t hesitate to reach out to your GP.
Thinking about getting an IUD? Book an appointment today to discuss your options and find the best contraception for you!